In a groundbreaking study, researchers have made a major breakthrough in the treatment of severe depression. By utilizing a unique deep brain stimulation (DBS) device, they have successfully identified a biomarker associated with signs of recovery in patients with treatment-resistant depression.
This innovative DBS device is not only capable of recording brain signals but also analyzing them using artificial intelligence tools. The study involved 10 adults with treatment-resistant depression, who received DBS therapy for a period of six months.
The researchers discovered a common brain activity signature or biomarker that correlated with patients reporting an improvement in their symptoms.
This exciting finding not only provides an objective method for tracking a patient’s response to DBS treatment but also offers hope for the development of more effective therapies for severe depression and other mental disorders.
Study Design
Enrollment of patients with treatment-resistant depression:
In order to investigate the efficacy of deep brain stimulation (DBS) therapy for treatment-resistant depression, the study enrolled 10 adults who had not responded to traditional antidepressant medications.
These patients were specifically selected due to the severity and persistence of their depressive symptoms, which made them suitable candidates for exploring alternative treatment options.
DBS therapy for six months:
The enrolled patients underwent DBS therapy for a period of six months. During this time, the DBS device was implanted in specific regions of their brains, and the therapy was carefully monitored and adjusted as needed.
This extended duration allowed for a comprehensive evaluation of the long-term effects and sustainability of DBS in managing treatment-resistant depression.
Biomarker Identification
Recording and analysis of brain signals using DBS device:
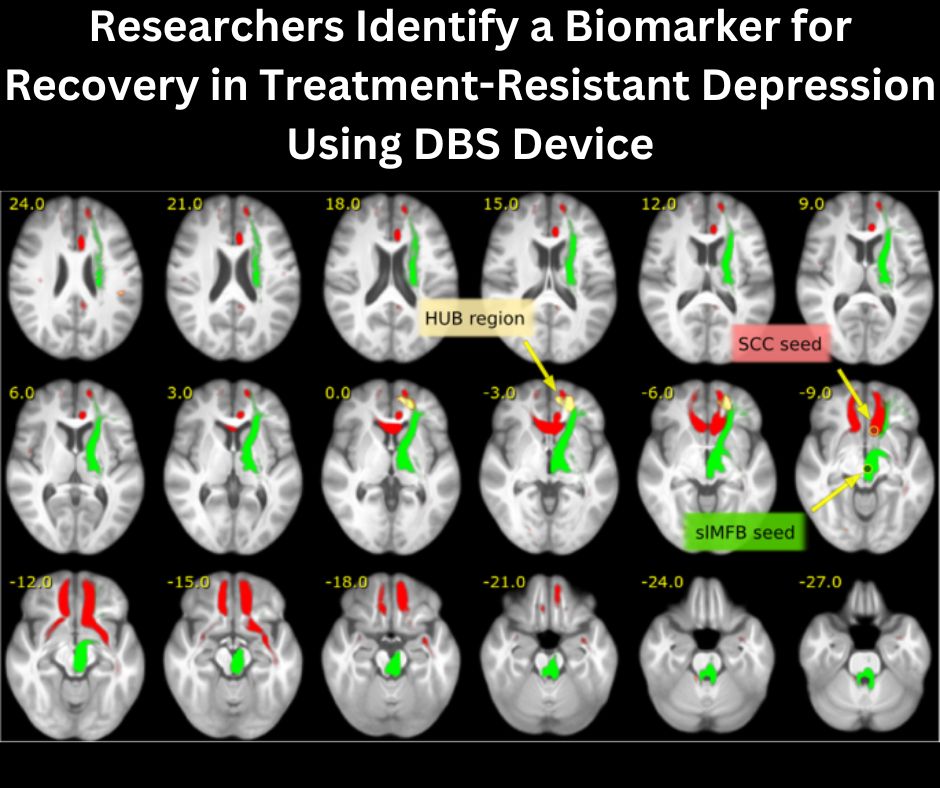
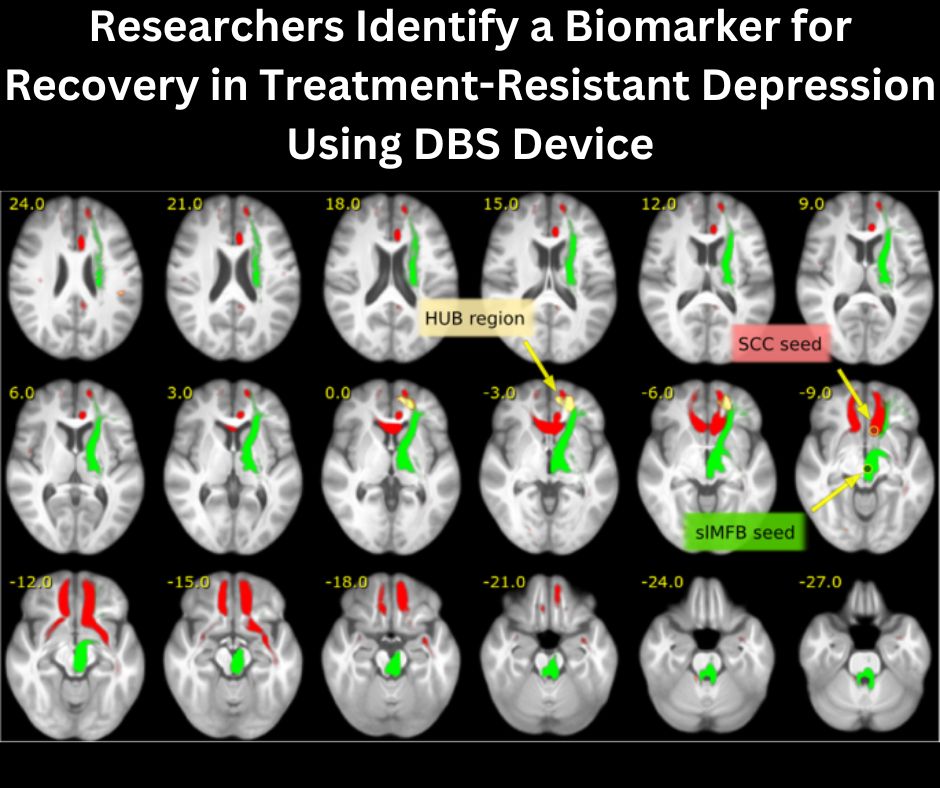
One of the innovative aspects of this study was the use of the DBS device not only for therapeutic purposes but also for recording and analyzing brain signals.
The device was able to capture detailed information about the neural activity of the patients while undergoing DBS therapy.
This provided researchers with invaluable insights into the underlying mechanisms of depression and how DBS affects the brain.
Correlation with patients’ self-reported symptoms of depression or stability:
By comparing the recorded brain signals with the patient’s self-reported symptoms, the researchers were able to identify a correlation or a common brain activity pattern that corresponded to different states of depression or stability.
This correlation served as the potential biomarker that could objectively measure a patient’s response to DBS treatment.
Objective Tracking of Response
Utilization of biomarker as an objective measure of response to DBS treatment:
The biomarker identified through the analysis of brain signals served as an objective measure to track the patients’ response to DBS treatment.
Instead of relying solely on subjective assessments, such as self-reporting of symptoms, the biomarker provided a more standardized and reliable way to evaluate the effectiveness of the therapy.
This objective tracking allowed for more accurate comparisons and assessments of treatment outcomes.
Possibility of making necessary adjustments based on biomarker:
Another advantage of using the biomarker as an objective measure was the potential for making necessary adjustments to the DBS therapy based on its indications.
By continuously monitoring the biomarker, healthcare professionals could identify any deviations or changes in the brain activity pattern and make timely and targeted adjustments to optimize the therapy for each patient. This personalized approach enhanced the overall effectiveness of the treatment.
Improvement in Depression Symptoms
Significant improvement in depression symptoms observed:
The study yielded promising results, with a significant improvement in the depression symptoms of the enrolled patients.
This positive outcome indicated that DBS therapy has the potential to effectively alleviate treatment-resistant depression and provide relief to individuals who have been struggling with severe and persistent depressive symptoms.
The response rate of 90% and 70% achieving remission or no longer being depressed:
The response rate to DBS therapy was exceptionally high, with 90% of the enrolled patients showing positive responses to the treatment.
Furthermore, an impressive 70% of the patients achieved remission or were no longer classified as clinically depressed.
These results highlight the effectiveness of DBS as a potential therapeutic option for those who have not responded to conventional antidepressant treatments.
Confirmation of Findings
Confirmation of findings in a second cohort of patients:
To ensure the reliability and validity of the initial findings, the research team is currently conducting a study with a second cohort of patients.
This replication of the study aims to verify the observed improvements in depression symptoms and the correlation between the biomarker and the patients’ self-reported stability.
Confirming these findings in a larger sample size will strengthen the evidence supporting the efficacy of DBS therapy for treatment-resistant depression.
Continued exploration of DBS for other mental disorders:
The success of DBS therapy in the treatment of treatment-resistant depression has prompted further exploration of its potential application for other mental disorders.
Researchers are now investigating the effects of DBS on conditions such as anxiety disorders, obsessive-compulsive disorder (OCD), and bipolar disorder.
By expanding the scope of DBS therapy, we can potentially provide new treatment alternatives for individuals who are not responding to traditional approaches.
Advancement in DBS Therapy
Significance of the study in early-stage DBS therapy:
This study represents a significant advancement in the field of early-stage DBS therapy. While DBS has been used for the treatment of movement disorders such as Parkinson’s disease for several years, its potential for mental disorders has not been extensively explored.
The successful application of DBS in the treatment of treatment-resistant depression opens up new avenues for research and treatment development in the field of mental health.
Potential application of DBS for severe depression and other mental disorders:
The positive outcomes of this study have paved the way for the potential application of DBS therapy in severe depression and other mental disorders.
By targeting specific brain regions involved in the pathophysiology of these conditions, DBS can offer a novel and potentially more effective approach to managing and treating mental health disorders.
This breakthrough has the potential to revolutionize the field of mental healthcare and improve the quality of life for countless individuals.
Importance of Biomarkers
The role of biomarkers in identifying recovery from treatment-resistant depression:
The identification of a biomarker related to clinical signs of recovery from treatment-resistant depression is a significant breakthrough in the field of mental health research.
Biomarkers play a crucial role in objectively measuring and evaluating the efficacy of treatments, especially in cases where subjective assessments may be prone to bias.
In the context of treatment-resistant depression, biomarkers provide clinicians with a valuable tool to track the progress of patients and make informed decisions about the appropriateness and effectiveness of interventions.
Potential for personalized treatment approaches:
Biomarkers also have the potential to revolutionize treatment approaches by enabling personalized medicine.
The unique neural activity patterns identified as biomarkers can help healthcare professionals tailor treatment plans based on an individual’s specific brain activity profile.
This personalized approach takes into account the heterogeneity of mental disorders and ensures that interventions are targeted and optimized for each patient.
By considering the unique characteristics of each individual, personalized treatment approaches can maximize the chances of successful outcomes and improve overall treatment efficacy.
Future Implications
Potential integration of biomarker monitoring into routine clinical practice:
The discovery and validation of biomarkers for treatment-resistant depression have profound implications for future clinical practice.
If successfully integrated into routine healthcare settings, biomarker monitoring can provide real-time feedback on treatment progress, allowing clinicians to make data-driven decisions regarding therapy adjustments.
This integration has the potential to enhance the precision and effectiveness of treatment, ultimately leading to improved outcomes and quality of life for patients.
Enhancement of treatment outcomes for depression patients:
By leveraging biomarkers as objective measures of treatment response, healthcare professionals can enhance treatment outcomes for individuals with depression.
The ability to accurately monitor and evaluate patient progress allows for timely interventions and modifications to treatment plans.
This proactive approach not only improves the efficacy of treatment but also minimizes potential risks and side effects.
Ultimately, the integration of biomarker monitoring into clinical practice has the potential to revolutionize the way we treat depression and other mental health disorders.
Limitations and Challenges
Potential limitations in the generalizability of findings to larger populations:
As with any study, there are potential limitations regarding the generalizability of the findings to larger populations.
The study’s sample size was relatively small, consisting of only 10 adults with treatment-resistant depression.
While the findings are encouraging and provide valuable insights, it is important to replicate the study using larger and more diverse cohorts to ensure the broad applicability of the results.
Additionally, factors such as patient demographics, comorbidities, and underlying biological variations may influence treatment outcomes and need to be considered in future research.
Challenges in implementing DBS therapy in clinical settings:
The implementation of DBS therapy in clinical settings poses several challenges. The procedure requires specialized surgical skills and expertise, limiting its availability to a select number of medical centers.
Moreover, the cost associated with the DBS device and the entire treatment process can be a barrier to widespread adoption.
Additional challenges include the need for long-term monitoring and support to ensure optimal outcomes, as well as the ethical considerations surrounding the use of DBS for mental disorders.
Addressing these challenges is essential for the successful integration of DBS therapy into routine clinical practice.
Ethical Considerations
Ethical considerations in the use of DBS for mental disorders:
The use of DBS therapy for mental disorders raises important ethical considerations that must be carefully addressed. While DBS has shown promising results in alleviating treatment-resistant depression, it is essential to ensure that ethical principles, such as patient autonomy, beneficence, and nonmaleficence, are upheld throughout the treatment process.
Informed consent, privacy protection, and a thorough understanding of the potential risks and benefits of DBS are crucial to ethically conducting mental health interventions.
Furthermore, ongoing monitoring and ethical review boards play a vital role in evaluating and mitigating any potential ethical concerns that may arise during DBS therapy.
Balancing Risks and Benefits in Treatment Decisions:
Balancing the risks and benefits of DBS therapy is a critical aspect of treatment decisions. While DBS has the potential to significantly improve the lives of individuals with treatment-resistant depression, there are inherent risks associated with brain surgery and the implantation of a medical device.
These risks must be carefully weighed against the potential benefits and the patient’s individual circumstances.
Transparency and open communication between healthcare professionals and patients are vital in ensuring that treatment decisions prioritize patient well-being and adhere to ethical standards.
In conclusion, the study on biomarker identification and the evaluation of DBS therapy for treatment-resistant depression represents a significant advancement in the field of mental health research.
The biomarker identified through the analysis of brain signals serves as an objective measure of treatment response, enabling personalized treatment approaches and potentially enhancing treatment outcomes for depression patients.
While there are limitations and challenges to overcome, the integration of biomarker monitoring into routine clinical practice has the potential to revolutionize the way we diagnose and treat mental disorders.
As the field continues to evolve, it is essential that we navigate the ethical considerations surrounding the use of DBS for mental disorders and strike a balance between risks and benefits in treatment decisions.
Ultimately, this research offers hope for individuals with treatment-resistant depression and paves the way for new possibilities in the management of mental health disorders.







